Sometime around 2010, about two-thirds of the way through his 13 years at the helm of the National Institute of Mental Health (NIMH)—the world’s largest mental-health research institution—Tom Insel started speaking with unusual frankness about how both psychiatry and his own institute were failing to help the mentally ill. Insel, runner-trim, quietly alert, and constitutionally diplomatic, did not rant about this. It’s not in him. You won’t hear him trash-talk colleagues or critics.
Listen to the audio version of this article:Feature stories, read aloud: download the Audm app for your iPhone.
Yet within the bounds of his unbroken civility, Insel began voicing something between a regret and an indictment. In writings and public talks, he lamented the pharmaceutical industry’s failure to develop effective new drugs for depression, bipolar disorder, or schizophrenia; academic psychiatry’s overly cozy relationship with Big Pharma; and the paucity of treatments produced by the billions of dollars the NIMH had spent during his tenure. He blogged about the failure of psychiatry’s Diagnostic and Statistical Manual of Mental Disorders to provide a productive theoretical basis for research, then had the NIMH ditch the DSM altogether—a decision that roiled the psychiatric establishment. Perhaps most startling, he began opening public talks by showing charts that revealed psychiatry as an underachieving laggard: While medical advances in the previous half century had reduced mortality rates from childhood leukemia, heart disease, and aids by 50 percent or more, they had failed to reduce suicide or disability from depression or schizophrenia.
“You’ll think that I probably ought to be fired,” he would tell audiences, “and I can certainly understand that.”
It was unsettling—as if the kindly captain of the world’s biggest ocean liner had sat down with his guests at dinner one evening and told them that their ship was unexpectedly lost and, if the crew could not soon correct course, they might well run aground, founder, and die.
Around this time, Insel told me recently, he’d just finished a talk describing the wonderful things the NIMH was discovering about the brain when a man in the audience said, “You don’t get it.”
“Excuse me?,” Insel said. “I don’t get what?”
“Our house is on fire,” the man said, “and you’re telling us about the chemistry of the paint. We need someone to focus on the fire.”
“I heard that,” Insel told me. “I went home and thought, There’s truth to that. It’s not just that we don’t know enough. The gap between what we know and what we do is unacceptable.”
For decades, most psychiatric research, and the NIMH’s in particular, had followed leads—clues about the brain’s hidden connections, the genome’s elusive secrets—that took decades to pay off. It was necessary work. But it had done far too little for those who were ill today.
Not long after that talk, at a conference in June 2015, Insel met Andy Conrad, who led Google’s new health spin-off, Verily. The two hit it off. That July, Insel visited Google’s Mountain View, California, headquarters. Conrad asked him: How would you like to run Verily’s new mental-health team? Instead of focusing on connections among neurons and genes, how about focusing on the connections between people that Google can track, analyze, and organize—the signals flashing across our world’s digital synapses—to better understand and treat mental illness?
Insel was in his mid-60s. Many people would have been thinking about retirement. But five months later, he had traded a kingdom of some 3,000 NIMH-funded researchers for a staff of one assistant, and he began working out of Google’s headquarters. He found in California’s digital culture a freedom he could previously only dream of.
“We are wildly ambitious,” he says. Insel hopes to use data—especially the rich, ongoing streams of data that a smartphone can provide—to detect a deteriorating state of mind faster and more reliably than we can now, and then to respond and turn things around more quickly. He believes a smartphone can be both a diagnostic instrument and, through the links it gives us to others, a life-saving mode of connection and treatment.
At any given moment, roughly one in seven of the world’s 7.5 billion people is struggling with mental illness. “We’re not going to reach all those people by hiring more psychiatrists,” says Insel. But we might reach them with smartphones.
Already, some 5 billion people worldwide have mobile phones. By 2020, it’s expected that 6 billion will use smartphones with the capability of capturing mental-health data and apps that can provide a form of treatment.
Insel wants to make those phones the central hub in a new way of delivering mental-health care. Former longtime colleagues speak of him the way baseball players speak of an ace pitcher who just signed with a rising franchise: I’m eager to see what he does.
Things always seemed to come easy to Tom Insel. His father, H. Herbert Insel, an eye surgeon in Dayton, Ohio, told him and his three brothers that they could do anything they wanted to as long as they became doctors first. As the youngest, Insel says, “I learned early on that the path to success was finding something others weren’t into.” He found his first niche outdoors, collecting crawly things that he kept in the basement. He did so well in school that when he was 15, he left high school and—without a diploma—entered a six-year B.A./M.D. program at Boston University.
Then, at 17, he did something that announced a pattern: Moving smoothly along an enviable track, he jumped off of it. With his bachelor’s work done and med school waiting for him, he got a year’s leave from the university; married his college girlfriend, Deborah Silber; and took off. They spent the 1969–70 school year skirting the Vietnam War, alternating stints of service work (a Hong Kong tuberculosis clinic for boat people; a Mennonite hospital in India) with travel around Nepal, Cambodia, and Thailand. Then he returned to Massachusetts, finished medical school and a year-long internship, took another year off to travel and study philosophy, and spent another three years in a psychiatry residency at UC San Francisco. After that, he presented himself, at age 27, for employment at the massive National Institute of Mental Health campus in Bethesda, Maryland.
Working in Bethesda as a research psychiatrist—increasingly studying patients, rather than treating them—Insel soon made a mark by running a drug trial that helped turn psychiatry away from talk therapy and toward chemistry. The trial showed that the antidepressant clomipramine helped people with obsessive-compulsive disorder faster and in more cases than psychoanalysis or standard talk therapy did. Today such a finding would go unnoticed. But this was the early 1980s, before Prozac and other selective serotonin reuptake inhibitors took over the world. At the time, OCD was seen as “the classic neurotic illness,” Insel recalls, Freudian anxiety run amok—“the prototype of what you got psychoanalysis for.” Yet Insel’s trial showed that a drug worked better and faster.
The papers Insel and others wrote about clomipramine over the next few years “really launched the field” of using antidepressants to treat OCD, he says, and helped pave the way for the Prozac era.
This irked some people. Freud may have been going out of fashion, but he still dominated psychiatry. His followers did not like losing to molecules. Insel hadn’t meant to stoke controversy. He liked Freud. That the drug became part of this turf war surprised him.
But as he followed up with other papers on the neurobiology of OCD, he soon found himself a leader in anti-anxiety-drug research. At 30, just three years into the job, he had his own research unit. “I could have just done drug trials for the next 20 years,” he says, “become a full professor, spent my time giving lectures and doing drug-company gigs.” Instead, he jumped the track. He closed his lab in Bethesda to study neuroscience at Johns Hopkins for a year, then returned to the NIMH. But rather than going back to Bethesda, he went to the sticks to work with one of the oddest people in neuroscience.
Surrounded by farm country, the National Institutes of Health’s facility outside of Poolesville—a scattered collection of low-slung labs, barns, and bare-bones offices an hour from Bethesda—was lonesome in a way that’s hard to find in Maryland. Even today, one route between there and D.C. involves a cable-guided ferry that crosses at a languid pace. It was sleepy. “I needed that,” Insel says. “I needed a place where nobody was around.”
The man he joined there, a renowned neuroanatomist named Paul MacLean, was, Insel says, “from another era.” MacLean, who died in 2007, had studied English literature at Yale and chemistry and physics in Edinburgh, Scotland, before getting an M.D. back at Yale in 1940. He loved brains. His lab was stuffed with drawers holding hundreds of micro-thin cortical cross sections, and with shelves holding “jars of formaldehyde,” Insel says, “with—I’m not making this up—roadkill.” Whenever MacLean came across something dead on the road, he’d put the carcass in his trunk and drive it to the lab. The idea was that one of his technicians would saw open the animal’s skull, snip its brain free of its spinal cord, and slice, stain, and mount some brain cross sections onto slides. MacLean would then compare the brain’s structure with that of other roadkill. He didn’t much care what kind. “He just wanted to see how, say, the hippocampus of a deer differed from that of a possum.”
MacLean named his lab the Laboratory of Brain Evolution and Behavior. “No commas,” notes Insel. “Syntax entirely unclear, so you could read or say it any way you wanted.” Insel had “almost complete freedom,” of a sort you can’t really get now.
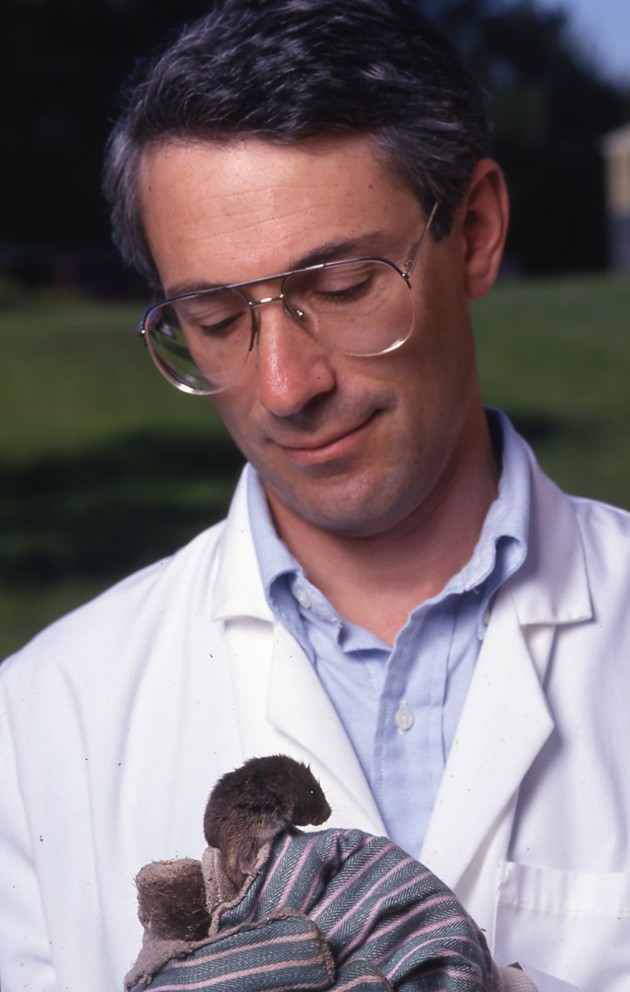
Insel’s landmark work was a run of vole studies that he started at Poolesville in the late 1980s.
Voles are rodents, mouselike but rounder, that live in burrows. In the ’70s, an ecologist at the University of Illinois at Urbana-Champaign named Lowell Getz was trapping small mammals in the Midwest for a population census. He kept catching one particular vole species—the prairie vole—in pairs. This was odd. Voles, like most rodents, generally show up in traps alone. But one out of 10 times that Getz caught a prairie vole, he caught a couple—a male and a female.
In a string of work requiring several years, much trapping, and many papers, Getz established that prairie voles were monogamous. This monogamy distinguished them from most of the other 150 vole species and, for that matter, about 95 percent of all other mammals. Most voles, for instance, mate and then stay together only minutes (or less) before moving on, and males pay little heed to their pups. But once a pair of prairie voles mates—an event typically triggered when a young female licks the urine of a male—they generally stick together till death. They cuddle and groom each other, and they cooperatively raise up to four litters a year. When one of the pair dies, the survivor generally foreswears all other voles.
Getz and Sue Carter, a behavioral endocrinologist, had already identified some of the hormones that drove prairie-vole monogamy. Insel and his lab picked up this thread. In one experiment after another, they outlined the genetic, molecular, and neural mechanisms that led to the prairie vole’s distinctive family life. Collaborating first with Carter and then mostly with his own colleagues Zuoxin Wang and Larry Young, Insel eventually showed how certain genes made the prairie-vole brain especially sensitive to two hormones, oxytocin and vasopressin, that surged at key times in a vole couple’s romance. Their work got heavy, often breathless press, which dubbed oxytocin “the love hormone.”
Their best work was astoundingly clever. For instance, by finding ways to bypass or silence some of the genetic signals and neurochemical receptors involved in the voles’ behavior, Insel, Wang, and Young proved the function of those signals and receptors. They’d identify, say, a gene that coded for an oxytocin receptor in the brain and delete the gene in an animal. With the receptor gone, the bonding behavior would disappear. Thus they turned speculative hypotheses into demonstrated findings. They showed that one could lay bare the biology of behavior.
The vole work made the careers of Insel, Wang, and Young. It also helped psychiatry with two perennial problems tormenting the discipline.
Psychiatry has always struggled to be taken seriously as a science. By the 1980s, the field seemed especially lost. Its best drugs were from the 1950s and ’60s. Most of its hospitals, their failings made infamous by works such as Sylvia Plath’s The Bell Jar and Ken Kesey’s One Flew Over the Cuckoo’s Nest, had been closed. Talk therapy, which often works, but by psychobiological pathways painfully difficult to discern, was frequently lampooned.
For these and other reasons, including its penchant for savage infighting, psychiatry in the ’70s was “a collection of diverse cults rather than a medical science,” as Melvin Sabshin, a onetime medical director of the American Psychiatric Association, later put it.
The field was also trying to adjust to one of the 20th century’s long, slow pendulum swings between environmental and biological explanations for behavior. In the century’s opening years, behaviorism was dominant in the wider culture, casting environment as the key variable in how people behaved; change a person’s environment, it was argued, and you’ll usually change his or her behavior. By the 1930s, the new science of genetics had bolstered the view that genetic (and thus presumably innate) differences were a crucial variable. After the Nazis exploited this view to help justify murdering 6 million Jews and hundreds of thousands of people with mental illnesses, the pendulum swung back the other way, toward the notion that a stressful environment could create social, educational, and mental-health deficits. Lyndon B. Johnson’s War on Poverty funded studies on the environmental roots of crime, minority-group mental health, and urban discord.
By the 1980s, however, this emphasis on the environment had come to be seen as misguided and overdone. It became harder to attribute schizophrenia or autism to emotionally cool “refrigerator mothers,” or youth violence to poverty.
These forces, then—the pressure for credibility, the swing toward biology as destiny—encouraged psychiatric research to focus less on environment itself and more on the biological mechanisms that responded to it.
Insel’s vole studies did precisely that. They were not the only works to do so, but they were among the earliest, cleanest, and most publicized. Beginning in the mid-’90s, Insel’s work took a place amid a handful of other new studies of social species, such as honeybees, songbirds, and cichlids (a fish), that showed how chains of neurobiological events produce fascinating and sometimes bizarre behaviors involving everything from mating and murder to language acquisition and social dominance. These studies did not really ignore environment. Rather, they explored the interplay of biology and environment by focusing on the former. And while these studies did not involve humans, they often explored humanlike behaviors.
These studies were exactly what psychiatry needed, offering to make it a discipline of numbers, mechanisms, circuits, and chemicals. The power of such work was almost certainly one reason Insel would later become the director of the NIMH. He came to represent a new way to explore behavior.
But first he had to get fired.
“What’d you do?,” I asked Insel when he told me he got sacked.
“It wasn’t what I did,” he said, smiling. “It was what I didn’t do”—focus directly on humans.
When Insel started the vole work, in the late ’80s, the NIMH did not yet consider animal studies of basic behaviors likely to reveal much about human mental health. Insel’s decade of work on family and social bonds in animals had done little to change that. “You’re talking about why a mother rat takes care of its baby?” says his former colleague Larry Young. “It was too fluffy.” So in 1994, three years after Insel published his first vole paper, he got canned.
Getting fired, Insel says, “was actually the best thing that ever happened to me.” It got him to see the importance of telling a clear story with his research, which proved essential in making that research successful. And it let him take another job that ultimately paved the way for his return to the NIMH as director.
Just weeks before Insel got fired, the famed Yerkes National Primate Research Center at Emory University had offered him an interview for the job of director. Insel, studying voles in Poolesville, figured he had no real shot at it. But by the time of the interview, he was newly fired, highly prepared, and keenly focused. He got the gig.
Insel spent eight years at Emory. While there, he worked with Wang and Young to expand their vole research into the magnum opus it became.
Running the primate center, meanwhile, gave Insel “a chance,” he says, “to understand how to build programs, how to build institutions, how to mentor, how to help people grow within an institution.” His changes at Yerkes upset some primatologists and drove some of them away. Yet he managed to get people to follow him, says Young, “not by force, but by being a nice guy and instilling excitement in others.” Insel showed that he could take the helm of an institution and change its course without causing mutiny.
In his 13 years as the director of the NIMH, from 2002 to 2015, Insel would become one of the best-known directors the institute ever had. His renown came partly from the length of his tenure, second only to the 15-year run (1949–64) of the founding director, Robert Felix.
When he became director, he took custody of a gluttonous giant that was being forced to diet. In the previous two decades, the institute’s budget had effectively tripled. But when Insel arrived, George W. Bush’s administration had just cut taxes and entered one war; it was preparing to enter another. Insel would work his entire tenure with an essentially flatlined budget—one in which, furthermore, 70 percent of each year’s expenditures was determined by prior commitments to ongoing programs.
If Insel wanted to change things, he would have to do so slowly, and he did. He devoted more research to the most-serious mental disorders, such as major depression, schizophrenia, and bipolar disorder. Anticipating that pharmacology would produce few effective new psychiatric drugs, he cut NIMH involvement in drug trials. And when, in 2010, he decided that psychiatry’s official diagnostic categories in the DSM no longer served the NIMH’s needs well, he spoke against them. In 2013, he rejected the DSM as a research guide, even though doing so infuriated many in the psychiatric establishment.
Throughout his tenure at the NIMH, Insel explicitly defined mental disorders as brain disorders. Critics of this approach expressed several complaints. Allen Frances is one of the world’s most prominent psychiatrists. He led an overhaul of the DSM in the early 1990s, producing its fourth edition, and has since become a vocal critic of psychiatry’s medicalization of normal distress, of its overuse of drugs—and of what he calls the NIMH’s overly brain-centric view of mental health.
“I think very highly of Tom Insel,” Frances says. “Right motives, decent guy, very smart, honest. But what he did at NIMH is disastrous. He inherited an institution that was already moving to a narrow, bioreductionist view of mental illness, and he moved it even further.” The translational jump from basic science to treatment is big in most of medicine, Frances says, but it’s especially big in psychiatry because the brain is the most complicated thing in the known universe. “Tom was naive about that. It’s not clear that any one patient, even today, has been helped by the neuroscientific advances made under his tenure.”
Almost all medical research faces the same challenge: striking the right balance between basic research (how does this work?) and translational research that converts the basic findings into treatments (how can we make this work differently?). To Frances and many other critics, the NIMH had that balance wrong, focusing too heavily on basic neuroscience research.
Another criticism leveled by Frances and others is that defining mental disorders as brain disorders underplays what psychiatrists call the psychosocial nature of mental states and mental health—the countless dynamics in social relationships that affect our psyches. A reductive biological model arguably neglects, for instance, the growing evidence that social isolation aggravates mental illness, while social support ameliorates it. Trying to understand mental illness without accounting for the power of social connection, this line of thinking goes, is like studying planetary motion without accounting for gravity.
Likewise, defining mental illness as a brain disorder shortchanges the role played by environment in general. Mental illness often occurs when a vulnerable psyche faces stress—sometimes chronic, sometimes sudden and acute. Many brain and large-scale genomic studies ignore this because the researchers don’t think environment is important, or because it’s hard to parse environmental effects into measurable components. Either way, a key element of mental health and illness can go overlooked.
Insel and his defenders say he did his best to respond to these problems. They note that he pushed NIMH research to yield more help faster for the sickest patients, and that he funded plenty of research on environment, behavior-based therapy, and social connection.
E. Fuller Torrey is a psychiatrist who worked at the NIMH in the 1970s and then became one of its fiercest critics as its emphasis increasingly focused on basic neurobiology in the 1990s. He was not thrilled about Insel’s appointment. “He’d worked on voles,” Torrey says. “My expectations were low.”
Torrey, among those who called loudest for the NIMH to generate not just findings but treatments, had developed a metric to tally what percentage of NIMH studies stood a reasonable chance of helping patients. When Insel took over, Torrey told me, that estimate stood at about 5 percent. Insel brought it up into the 20s.
“He did a yeoman’s job. I have nothing bad to say about Tom except that he didn’t stay longer.”
Insel never wavered from framing the institute’s mission as biological. When I asked him about this directly, he unambiguously defended the NIMH’s biocentric stance. But if you examine the later years of his tenure closely enough, you see signs of vacillation—of someone still believing something, but without as much conviction.
This comes across in his 2013 ted Talk. Insel—as at ease, confident, and disarming as ever—opens with his iconic graphs showing how psychiatry has gone nowhere for decades. Then, after telling the audience members that he can understand why they think he should be fired, he pivots to say, “I think we are about to be in a very different world as we think about these illnesses,” and describes the newest wonders the NIMH is discovering about the brain.
I keep going back to that talk because, right there on the ted stage, Insel seems to be of two minds. When he embraces his dismay and then sets it aside, I feel I’m seeing a person who is in the process of flipping his allegiance between two contradictory ideas. By the time of his ted Talk, Insel had ceased believing not just in the categories used to describe mental illnesses but in the magic of drugs or genomics to diagnose and treat them. He was essentially saying of psychiatry: We’ve fallen short of our promises for decades, but we’re finally figuring out the brain, so we’ll deliver. Yet even as he described the brain’s wonders, Insel seemed to understand that he was still talking paint chemistry, and not attending enough to the raging fire.
“Tom was very blunt” toward the end of his tenure, says Bruce Cuthbert, who worked alongside Insel at the NIMH and served for 10 months as the acting director after Insel left. “He was brave enough to say, ‘Actually, we don’t know much of anything at all that could help individual patients.’ ”
Insel is impatient. When he’d been at the NIMH, he told me recently, he’d thought of the results horizon as being 10 to 30 years out. But he is 65, and tired of waiting. “I want to make something happen in three years.” He told me this as we sat in the enormous, airy lobby of the new Verily building in South San Francisco. Early this May, as I was putting the final touches on this story, I emailed Insel to confirm and update a few things—and found that he was leaving Verily the next day. As small and nimble as Verily was compared with the NIMH, he said, he was now joining a far smaller outfit called Mindstrong Health, a start-up co-founded by three people—himself, Paul Dagum, and Richard Klausner—that would pursue an agenda much like the one he’d outlined at Verily.
“A similar path,” he told me.
Insel had jumped the track again.
Two weeks later I visited him at home in Pleasanton, California.
“I loved working at Verily,” he told me. It was only after he started there, he said, that he grasped the scale of ambition and possibility that today’s biotech landscape offered. He liked Verily’s CEO, Andy Conrad, whose brash, sometimes profane style has reportedly driven away some other top Verily employees. “It was hard to leave,” Insel said. But the features inevitable in a 500-person company (Verily) that was part of a 74,000-person company (Alphabet, Google’s holding company) made a smaller option look much better. “The speed bumps you have to go over to get something out the door,” Insel said, would now be fewer and lower.
As we talked, Mindstrong was remodeling offices in Palo Alto, an hour’s drive away. Insel said he plans to work most days from home, where he can have lunch with his wife, and where a garden, a pool, a chicken coop, and a 350-vine vineyard beckon out back. But Insel didn’t join Mindstrong for the barefoot commute. He likes his co-founders and the greater agility offered by what he calls “a ‘two pizza’ company—small enough to feed with two pizzas.” Currently Mindstrong has about a dozen employees. Talking to me on his second day as Mindstrong’s president, Insel told me he had already found it far easier to strike research partnerships with caregiver or insurer networks to test and refine the patient-monitoring systems that are at the core of the company’s plan. “We actually did one of those last week,” he said, “and the network will start collecting the data this week. We can just move much faster at this size.”
Mindstrong’s plan, much like that of Insel’s unit at Verily, is to use the smartphone’s powers to do two things that psychiatry hasn’t figured out how to do: easily detect early, or even predict, the onset of mental illness; and quickly get effective, affordable care to those who need it.
This idea has been floating around Silicon Valley and mental-health circles for several years. Insel estimates that a good five or 10 other companies or research teams—including Verily—are trying to do something similar. Mindstrong hopes to gain an edge by combining Insel’s expertise and connections in the mental-health field with Klausner’s business experience and Dagum’s data-analysis tools and skills—and by moving quickly.
The force they hope to harness is the power of daily behavior, trackable through smartphone use, to reflect one’s mental health. As people start to slide into depression, for instance, they may do several of the following things easily sensed by a phone’s microphones, accelerometers, GPS units, and keyboards: They may talk with fewer people; and when they talk, they may speak more slowly, say less, and use clumsier sentences and a smaller vocabulary. They may return fewer calls, texts, emails, Twitter direct messages, and Facebook messages. They may pick up the phone more slowly, if they pick up at all, and they may spend more time at home and go fewer places. They may sleep differently. Someone slipping toward a psychotic state might show similar signs, as well as particular changes in syntax, speech rhythm, and movement.
Insel says such data provide “a more objective, textured picture of people’s lives,” one collected continuously, rather than just at weekly sessions. (A therapist, the joke goes, knows in great detail how a patient is doing every Thursday at 3 o’clock.) With inputs like these, a phone could sense the beginning of a crisis and trigger an appropriate response. Because this response would come earlier, it could be more measured, less jarring, and less medication-heavy. “The earlier you intervene, the better the outcomes,” Insel says. “Instead of detect and treat, it’s predict and pre-empt.”
Mindstrong has three patents for a data-collection-and-analysis system built roughly for such purposes. Dagum designed this system, which can harvest some of the smartphone’s scores of data streams.
How might MindStrong’s system actually work in practice? Insel points to two prototype examples.
The first is a company called 7 Cups, which Insel first learned about because his daughter works there. 7 Cups provides text-based peer counseling and support for people with depression or anxiety or a long list of other conditions. Registering for the simpler services, such as peer connection, takes only seconds, and users can also get referrals to either coaches or licensed mental-health counselors and psychologists.
According to the CEO, Glen Moriarty, 7 Cups serves a young, diverse demographic (90 percent are under the age of 35) that is likely to go underserved by traditional mental-health care. When Insel first heard about these demographics, he said, “a light bulb went off. This is about providing access for the first time”—and to people who don’t necessarily want to talk to a psychotherapist. They want to help each other. With a simple smartphone app and website, 7 Cups seeks to quickly and inexpensively connect such people while also providing a range of clinical support.
The company collects an astounding amount of anonymized data—a key to increasing its accuracy in detecting mental states, and to the efficacy of its response to signs of worsening illness. When 7 Cups told Insel that it gives everyone who registers the chance to take a standardized screening test for depression, anxiety, and stress, called dass‑21, he asked how long it would take to get him, say, 1,000 of those, scrubbed of identifying information.
“They said, ‘We’ll do 2,000 this afternoon. You want all of them, or what part?’ ”
A second rough model for Mindstrong’s approach is an app called prime, developed by Danielle Schlosser, a clinical psychologist whom Insel recruited to Verily from the psychiatry department at UC San Francisco. prime (Personalized Real-time Intervention for Motivation Enhancement) was inspired partly by research showing that social connection and peer support can reduce the severity of depression and schizophrenia. Schlosser designed it for people ages 14 to 30 who’d been recently diagnosed with schizophrenia. It could be adapted for use by people diagnosed with or at risk for other mental disorders.
The heart of prime is a Facebook-like mobile app that connects members to both a circle of peers (in this case, others who have had psychotic episodes) and professional clinicians who can assist as needed. Currently about 50 people use prime at any given time, with at least five clinicians logged on and available. Most members use it daily. Members tell Schlosser they gain enormously simply by seeing that other members are perfectly normal people who happen to have schizophrenia.
The app has three real functions. One is connecting people so they can turn to one another for help, perspective, and affirmation. Another is providing a set of motivational essays, talks, and interactive modules that help with decisions and dilemmas common among the membership. The third is quickly spotting emerging crises and responding with peer, social-service, and clinician support.
Sometimes it works in more dramatic fashion. Schlosser describes one participant who, because he regularly conversed with people in the group, felt free to volunteer something he might not have if he were more isolated: He confessed that he was feeling a bit off, as if he might be sliding back toward psychosis. When Schlosser’s team reviewed his message history, it saw changes in syntax and language use that suggested emerging psychosis. His physician then tweaked his meds, and both his unease and his disordered syntax resolved.
A system like prime or the one used by 7 Cups, notes Insel, combines the two components necessary to any approach to mental-health care—assessment, by collecting and analyzing the data a person and his smartphone can provide; and intervention, which might include anything from informal social support to medical support (either inpatient or outpatient).
Mindstrong, he says, will first focus on assessment, spending the next year or so testing phone-based data-collection-and-analysis systems; and then explore ways to partner with others to provide intervention through what Insel calls “learning-based mental-health care.” Continuous assessment and feedback would drive the interventions. Likewise, all therapies would use measurement-based practices, which give clinicians and patients steady feedback on what’s working and what isn’t—an approach shown to sharply improve outcomes.
To preserve users’ privacy, Insel says, Mindstrong will collect information only on an opt-in basis, and all data will be strongly encrypted. For most services, Mindstrong will save not actual data streams, such as what is said in spoken or typed conversations, but only metadata that reflect state of mind without revealing actual conversation. This might include semantic structures or the repeated use of key words or phrases that can reveal emotional or cognitive states such as depression, mania, psychosis, and cognitive confusion. All data will be firewalled according to strict patient-privacy practices.
Even such metadata, of course, might make an attractive target for people who’d want to exploit it. (Picture a digital-era version of the Nixon administration’s bungled attempt to steal the psychiatric records of Daniel Ellsberg, who leaked the Pentagon Papers, so that it could blackmail or smear him.) The only thing stopping such an effort in digital form might be the strength of Mindstrong’s firewall or its willingness to defy a government request for data. This danger is real. Google, for instance, has steadily reduced the proportion of government data requests it responds to, but in the second half of 2016, the company reports, it still produced data for 60 percent of such requests overall, and 79 percent of such requests from the U.S. The company reveals little to the public about which requests it honors or why. For these reasons, some digital-privacy experts think it’s dangerous for any company to collect and keep something as sensitive as psychiatric-patient data. For his part, Allen Frances feels it’s naive to trust any commercial entity to permanently protect such data from other commercial interests, hackers, or a government bent on getting the information. Others argue that this worry is itself naive, since most of us already leave enough footprints with smartphones, computers, phone calls, and credit-card purchases to forfeit the privacy Frances wants to protect. The question may not be whether a Mindstrong firewall would be perfect, but whether it would be stronger than the many porous containers already holding our personal and medical information.
I once asked Insel how he saw his move to Silicon Valley in relation to the rest of his career. I expected he’d say it was a complete departure.
Instead he said it felt to him like a return to his first concerns—“a return to behavior.” He meant the voles.
The fundamental assumption behind the vole work, and behind Insel’s career at the NIMH, was that beneath behavior lay biological mechanisms you could discern and then tweak to change that behavior. The crux of the biological model, in other words, was that you could and should address mental illness from within. Otherwise, why bother with the nearly impossible job of figuring out how it all worked? You looked for mechanisms so you could fix the machine.
Now, however, Insel means to address mental disorders not from the inside, but from the outside; and not with something new, but with things at hand. He’s shifting from mechanistic discovery to practical application. He is acting on the epiphany he had when the man at his talk complained that Insel was discussing paint chemistry when he should have been putting out fires. It was then, Insel says, that he began “to realize that the really urgent issue isn’t that our treatments get better, but that we don’t use what we have today.”
Insel will always believe in the value of research, of figuring out how things work. But our most pressing problem, he says—what keeps psychiatry from making the huge strides that have been made in disciplines like infectious disease and cardiology—“is not what we don’t know. We know well enough what works. Our problem is that we’re not doing it.”
The other big development in Insel’s work today is his embrace of social contact as a basic health necessity. For this he credits Schlosser’s work. “She convinced me that people with psychotic illness really crave social connections,” he said. “This was a great wake-up call for me: to see they want to connect on their own terms, sometimes anonymously, on their own schedule, in a way that they feel they can control”—often with others like them, in relationships that feel equal, rather than only with clinicians who may seem to hold too much power.
Why didn’t he come to all this sooner? Why now?, I asked.
“I have always believed,” he said, “that to get the most impact, you should go where you get the most traction.” Even five years ago, he said, he could not have gotten traction on the ground that he and Mindstrong are working today. Smartphones weren’t ubiquitous enough; the data weren’t rich enough.
“But now,” he said to me, “now we can do this.” He was leaning forward and smiling and holding both hands up in front of him as if he were fixing to catch something—as if he were a basketball player who’d just shook his defender and was calling for the ball to take an open shot. His eyes had the look of someone who felt he couldn’t miss.